Below are a number of surgical cases with before and after pictures with a short explanation. All images were used with permission and all patient information has been removed.
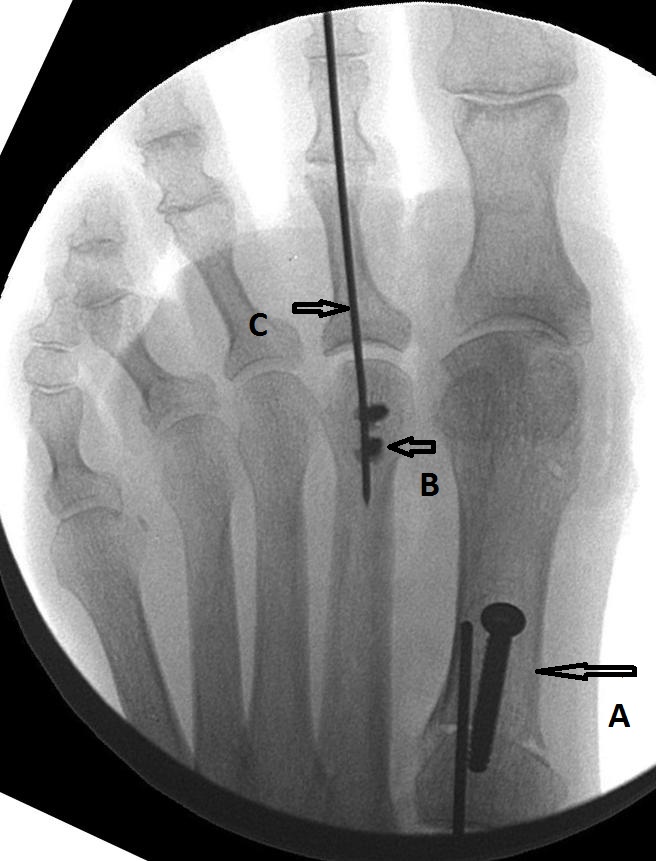
Bunion and Hammertoe Correction:
- On the left is the before x-ray and on the right is after surgery.
- The red A arrow shows how a bunion forms as this long bone slowly moves the direction of the arrow dislocating the big toe joint over time.
- The bunion is fixed by cutting the bone at black arrow “A” and pivoting the long bone towards the 2nd toe. It is held in place by a pin and a screw. The hammertoe is fixed by cutting the bone at red arrow “B”, shortening the long bone and then fusing the nearest joint in the toe with a pin.
- The long pin in the 2nd toe (arrow C) is pulled out after 4-6 weeks as it is only temporary to allow for the toe tissues to heal in the correct position. The remaining hardware stays in place and usually does not need to be removed.
- This is a case from residency. I do not do this type of bunion correction because of its inherent instability if a patient steps on it too early (black A arrow). It is an option however if needed.

- Here is a typical bunion correction: often called an “Austin Bunionectomy”. One or two screws are all that is needed. This type of bone cut and fixation allows the patient to walk early as soon as tolerated.
- If the bunion is more severe then bone cuts must be made at either of the above black arrows with the bottom arrow signifying removal of that joint should it be very flexible.
-
Above is an example of a Lapidus Bunionectomy. This is an option when hypermobility of the joints is suspected or the deformity is very large.
- The patient above had a hammertoe and bunion deformity that another surgeon had tried to fix with an Austin bunionectomy, when the more appropriate surgery would have been a Lapidus or similar procedure seen on the left.
-
Some patients require fusion of joints such as in rigid contracted hammertoes and arthritis of joints as above. The pin in the 2nd toe will be removed at 6 weeks.
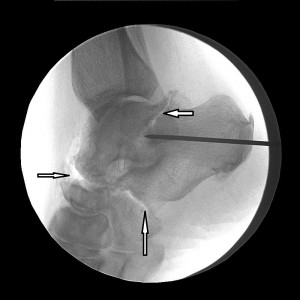
Foreign Bodies:
- As you well know, anything and everything has tried to force its’ way into the human foot. Often times, surgery is needed to extract the object in a sterile environment followed up with antibiotics and monitoring for possible infection. Always check your tetanus shot status.
- Take a guess. 16 penny framing nail. This went through a boot trapping leather, sock etc against the skin. High risk for infection.
- If you’re thinking, “that looks like the eye of a needle” you’d be right. The patient didn’t even know it was in their foot. This x-ray was taken for a totally different reason. Diabetics beware, the numbness that often accompanies this disease can set you up for disastrous consequences. Check your feet morning and night. Call your podiatrist with the smallest concerns. This could have ended in infection and amputation. Very lucky patient.
- You’ll never guess. That’s part of coral reef, poisonous barbs and all. Came out nicely in the end.
Toe Implants:

- Anything look wrong here? This young avid runner came in with a story of receiving this implant years before by another doctor after the joint became arthritic. The patient felt a pop while running and had caused the implant to fracture through the bone. The joint had to be remodeled and fused. Toe implants are still not panning out for athletic and active individuals so beware if your doctor recommends one and you have goals of running and jumping. If you do, you’re probably are not a good candidate. Toe implants have been shown to work reliably only in sedentary and less active individuals. Even with the best patients, the toe implants longevity is not much better than 5-10 years. If you are young, we can remodel the joint, if that fails, joint fusion is a very viable standard that allows for full activity believe it or not.
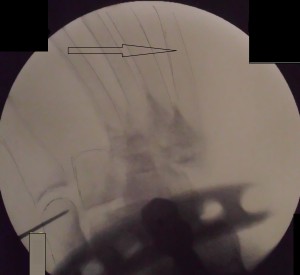
Charcot Reconstruction:
- This image didn’t come out very well, but if you look close the four metatarsals are dislocated off the foot (see the arrow). Charcot neuroarthropathy is a catastrophic disease state most often associated with diabetes where the bones and joints become soft and crush and/or dislocate. This deformity requires major reconstructive surgery to create a foot that can fit into a shoe and prevent ulcers from forming from pressure points.
- The most recent philosophy wave to go out through the foot and ankle community is large external fixators, a number of which I have learned how to do. These are falling out of favor however with large numbers of patients experiencing deformity re-occurrence.
- We are now showing much better results with a method called “ladder plating”. See below. The idea is very basic, as the bone begin to harden we reconstruct the foot and place a large number of screws that lock into a plate into the foot creating a rigid construct that prevents further dislocation should the disease strike again. The gaps you see in the joints to be fused were filled with a bone graft that increases the chances of bony union and will later fill in with bony material.
Mid Foot Fractures:
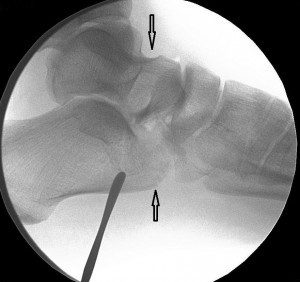
- The black arrows show where fractures occurred across the talus (bottom of the ankle joint) and calcaneous (heel bone).
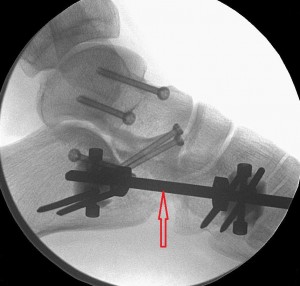
- The red arrow indicates the hardware that was later removed. The lighter colored screws are left permanently. The dark colored frame protrudes through the skin and is left in place for 6 weeks or so. We took this approach because the calcaneous was so crushed it had to be held out to length to allow proper healing.
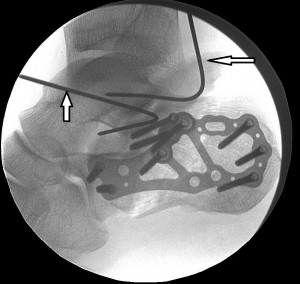
- This is a pretty nasty calacenal (heel bone) fracture. These are a life changing event because surgery is often fraught with complications because of poor blood flow to the area. Often even if the calcaneous is successfully put back together, the surrounding joints become arthritic because of the multiple insults to those joints.
- The large plate and all the screws remain initially. The two arrows indicate temporary wires that are removed at the end of the surgery.
Arthritis and Joint Fusions:
 The three white arrows above indicate advanced osteoarthritis. The current standard of practice is to fuse these joints to remove the painful “bone on bone” motion.
The three white arrows above indicate advanced osteoarthritis. The current standard of practice is to fuse these joints to remove the painful “bone on bone” motion.
- The above procedure is the final product. Three joints were fused. This is called a “Triple Arthrodesis”.
Ankle Fracture:
 This is a typical ankle fracture (see red arrows) that often results from falls involving twisting motion at the ankle.
This is a typical ankle fracture (see red arrows) that often results from falls involving twisting motion at the ankle.
- Often the fibula is fractured and requires a long plate because it is such a thin and weak bone. The tibia is more robust and can be fixed normally with screws and pins.
















Gross!
My SIL had a needle go clean into her foot, but her doctor couldn’t find it to extract it. It worked itself out again years later.